Cancer treatment has long been a complex battleground, with researchers exploring diverse avenues to combat this relentless disease. A pair of groundbreaking studies sheds light on novel strategies to leverage the immune system’s dual responses, challenging previous assumptions about immune functionality in cancer therapy. As these studies illuminate the potential of synergizing immune responses, they signal a transformative shift in the cancer treatment landscape.
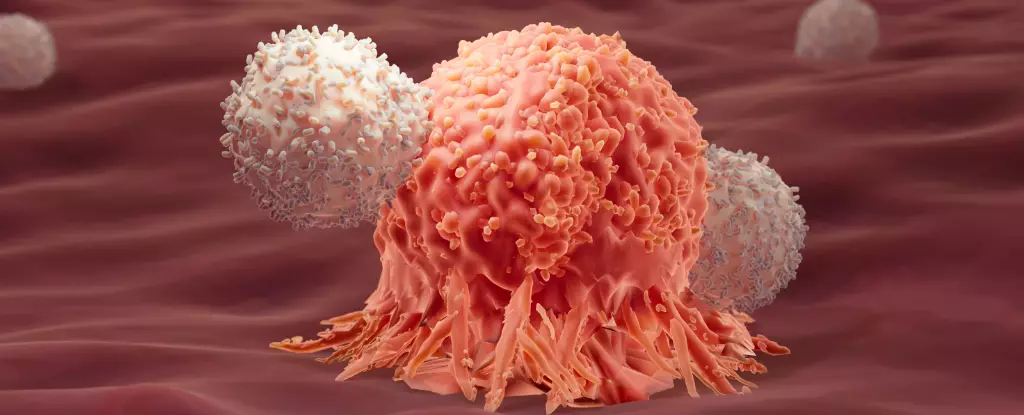
Traditionally, the focus in cancer immunotherapy has centered on optimizing Type 1 immune responses, known for their effectiveness against intracellular threats, such as malignancies. However, new research proposes that Type 2 immune responses—previously dismissed as less relevant or even negative in the context of cancer—might have a crucial role in long-term remission. This revelation comes from an extensive examination of clinical data from patients benefiting from CAR-T cell therapy, a promising immunotherapy strategy that enhances the body’s own T cells to more effectively locate and obliterate cancer cells.
Researchers from École Polytechnique Fédérale de Lausanne (EPFL) meticulously analyzed genetic data from nearly 700,000 CAR-T cells sourced from 82 patients who underwent treatment for acute lymphocytic leukemia (ALL). Among these, survivors who maintained remission for over eight years exhibited distinct markers associated with a Type 2 response. The conventional notion was that this type of immune reaction, which generally tackles larger threats like parasites, was irrelevant or even detrimental to tackling cancer. However, the correlation between survival and Type 2 markers calls for a paradigm shift—a reconsideration of the immune interplay in the battle against cancer.
The second study investigated how combining both immune response types could amplify treatment efficacy. Conducted on mice with colon adenocarcinoma, researchers compared the outcomes of conventional Type 1 treatment against a hybrid approach incorporating a carefully engineered Type 2 response. The results were striking: a remarkable 86 percent cure rate in the combined response group as opposed to none surviving in the Type 1-only group. Such findings are particularly compelling given that solid tumors typically demonstrate resistance to singular immunotherapy strategies.
Upon closer examination, the modified Type 2 immune proteins were found to enhance glycolysis—a metabolic pathway crucial for T cell energy metabolism. This enhancement appears to stave off T cell exhaustion, a significant factor in the immune system’s ability to combat persistent cancer cells effectively. The synergy observed between the two immune responses—akin to “yin and yang”—suggests a collaborative dynamic where each response enhances the other’s efficiency.
As promising as these findings are, researchers caution against overinterpretation. While a noteworthy correlation exists, the studies do not definitively establish a causal relationship between Type 2 immune responses and long-term remission. Future investigations will be critical to unraveling this potential linkage. Nonetheless, this dual-response approach opens an exciting reparability for broader immunotherapeutic applications beyond leukemia, particularly for patients with solid tumors who have historically faced bleak prognoses.
These advancements highlight the urgent need for personalized cancer treatments. By identifying specific immune profiles, oncologists could tailor therapies to exploit patients’ unique immune landscapes, maximizing treatment effectiveness. This precision-based approach could transform how immunotherapy is delivered, shifting from a one-size-fits-all model to one that adapts to individual immune characteristics.
The studies serve as a powerful reminder of the complexity and resilience of the immune system in the face of cancer. The traditional binary view of immune responses may need reevaluation, as the collaborative power of these responses emerges as a compelling avenue for enhanced cancer therapies. The future of cancer treatment may lie in embracing this sophisticated interplay of immune mechanisms, offering new hope for those grappling with this prevailing health challenge. As research progresses, it is crucial to continue exploring these dimensions to unlock innovative therapies that could significantly elevate patient outcomes in the fight against cancer.