Recent advancements in medical research have unveiled exciting potentials for extending the window of time in which resuscitation can successfully restore brain functionality after cardiac arrest. Scientists in China have made groundbreaking strides by demonstrating that brain activity in pigs can be reinstated even up to an hour after clinical circulation has halted. This promising discovery paves the way for new methodologies aimed at enhancing the prospects of survival and recovery for patients experiencing sudden cardiac arrest.
Sudden cardiac arrest remains one of the most critical medical emergencies, leading to immediate and severe consequences due to the abrupt stop in blood flow. The resultant ischemia—the deficiency of blood supply to organs—primarily jeopardizes brain health, with irretrievable damage potentially occurring within mere minutes. The short timeline for resuscitation highlights a crucial challenge in emergency medicine, necessitating innovative approaches to extending this timeframe to improve patient outcomes.
Researchers have known for some time that the interplay between multiple organs during ischemic events plays a pivotal role in the likelihood of brain recovery post-cardiac arrest. Yet, the specific impacts of individual organs have largely been uncharted territory until recently. This necessitated a more focused study on how organ interactions affect brain recovery, leading to the unearthing of new therapeutic possibilities.
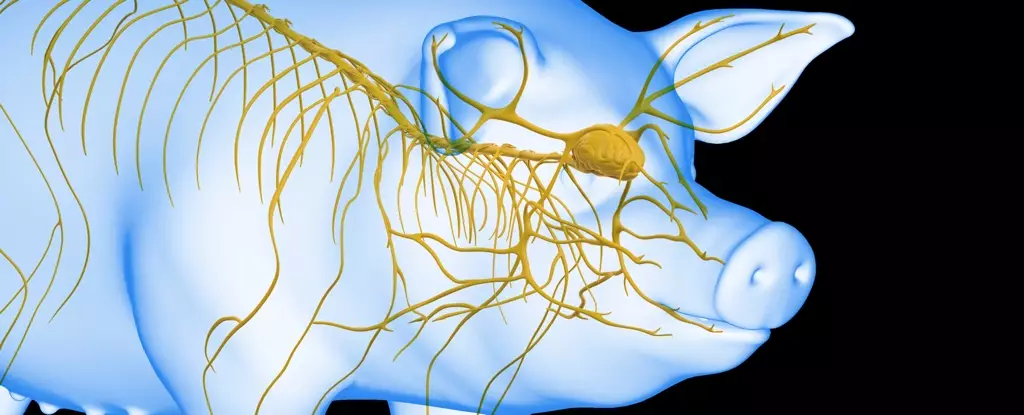
A dedicated team, led by Dr. Xiaoshun He from Sun Yat-Sen University, embarked on a series of experiments using Tibetan minipigs as their model organisms. These trials aimed to dissect the effects of including the liver—a crucial organ known for detoxifying blood—in the resuscitation process. By comparing two groups of pigs subjected to brain ischemia for 30 minutes, researchers observed disparities between those experiencing simultaneous liver ischemia and those that did not.
The results were telling. The pigs who suffered from isolated brain ischemia sustained significantly less brain damage than those who faced concurrent liver ischemia, underscoring the liver’s critical role in safeguarding neurological function during ischemic episodes. This highlighted the potential for functional liver integration in future resuscitation protocols.
The research escalated to its next phase as the team experimented with the integration of an undamaged liver into a life support apparatus designed for the revival of brain activity. This system, although primarily experimental and not directly translatable to human treatment yet, served as a vital tool in understanding how the dynamics of organ function influence recovery timelines.
The artificial heart and lungs setup allowed for the circulation of fluids through the brain, simulating conditions necessary for functional recovery. Initial experiments illustrated that when the brain was reconnected to the life support apparatus 10 minutes post-initiation, electrical activity returned within a half hour before gradually waning. However, the presence of a functioning liver significantly altered outcomes.
Further exploration revealed that reconnecting at 50 minutes post-ischemia yielded the most auspicious results. The pigs’ brains exhibited sustained electrical activity for up to six hours, elucidating a critical delay period after ischemia where the integration of a healthy liver proved to be remarkably beneficial.
Most notably, the research conveys vital implications for enhancing survival and rehabilitation prospects for patients experiencing cardiac arrest. The evidence garnered suggests a fundamental relationship between liver functionality and brain recovery post-ischemia, thereby prompting a reevaluation of current resuscitation protocols.
As scientists dissect these complex interactions further, novel strategies could emerge, transforming emergency medical practices. The insights gleaned from these animal models promise more than just an academic discussion; they hold the potential to revolutionize how clinicians approach the challenge of brain injury prevention during critical care scenarios. While the transition from laboratory findings to clinical adoption may involve significant hurdles, the ongoing dialogue surrounding this research is bound to spark innovation.
The study of pig brain recovery following cardiac arrest marks a significant milestone in understanding the multifaceted relationships between organ functions during critical emergencies. By tapping into the protective roles of key organs such as the liver, researchers are beginning to unveil a pathway toward extending the resuscitation window and improving outcomes for patients. As experiments continue to unfold, the promise of a future where brain damage from cardiac arrest can be mitigated grows ever closer, representing a monumental leap toward enhanced medical care.