Lung diseases are among the leading causes of mortality globally, claiming millions of lives annually. The complexity of these conditions, such as chronic obstructive pulmonary disease (COPD) and cystic fibrosis, is compounded by a severe shortage of viable treatment options and donor organs for transplantation. With the inadequacies of current animal models, researchers are in urgent need of innovative solutions to better understand and treat these debilitating diseases. A groundbreaking development from a recent study published in ACS Applied Bio Materials introduces a mucus-based bioink, potentially paving the way for more effective experimentation and therapies in lung health.
For individuals grappling with chronic lung conditions, treatment often involves the management of symptoms through medications rather than addressing the root causes. Despite advancements in medical science, a definitive cure remains elusive. Currently, the dominant approach involves pharmacological interventions; however, these often fail to provide a holistic solution. Many treatments are tested on rodent models which, while useful, do not accurately reflect the multifaceted nature of human pulmonary diseases. The gap between animal-based research and human application reveals a critical need for alternative methods to understand lung conditions.
In the quest for better research models, bioengineers have turned their attention to the potential of producing artificial lung tissues in laboratory environments. The concept of using 3D bioprinting to create tissue-like structures offers a promising pathway. However, the difficulty lies in finding suitable bioinks that can effectively support cell viability and mimic the characteristics of human lung tissue. Herein lies the innovation presented by Ashok Raichur and his team—the introduction of a mucus-derived bioink specifically designed for 3D printing lung tissues.
This pioneering research began with mucin, a principal component of mucus, which has not received extensive attention in bioprinting applications. Mucin’s molecular structure is reminiscent of epidermal growth factor, a vital protein that promotes cellular attachment and proliferation. The researchers chemically modified mucin with methacrylic anhydride to create a compound known as methacrylated mucin (MuMA). By combining MuMA with lung cells, they established a novel bioink that showcases promise for pulmonary applications.
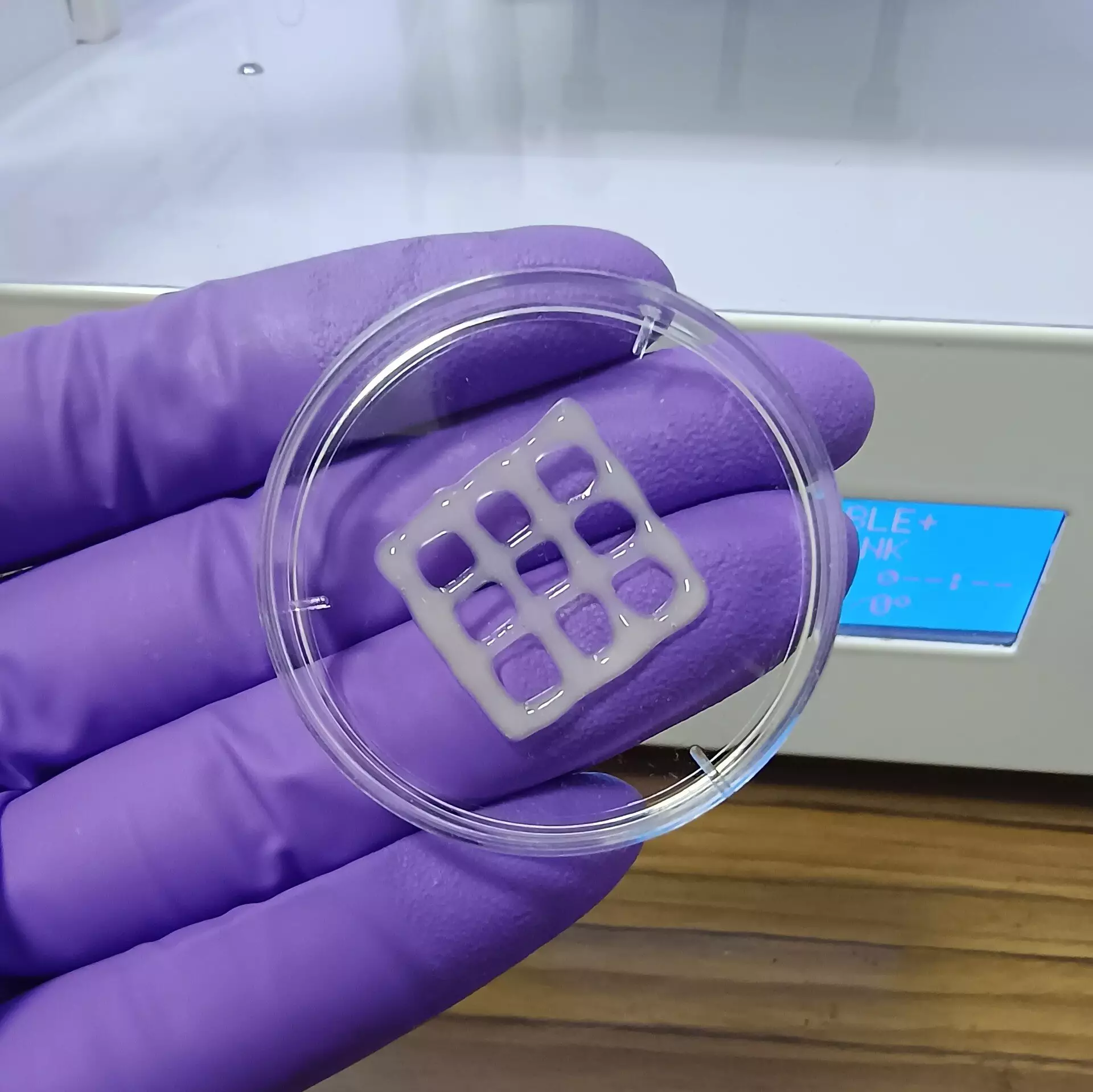
To enhance the properties of the bioink, hyaluronic acid was integrated into the formulation. This naturally occurring polymer boosts viscosity and fosters cell adherence, crucial for the subsequent growth of lung tissue. Once the bioink was prepared, the researchers conducted 3D printing with various test patterns, producing intricate structures that resemble lung architecture. The application of blue light initiated a crosslinking process, stabilizing these structures into a porous gel.
The resulting gel displayed remarkable characteristics essential for supporting cellular life. With interconnected pores, the structure allowed for the diffusion of vital nutrients and oxygen, simulating the physiological environment required for lung cells to thrive. Through careful observation, the researchers concluded that these printed constructs were biocompatible and exhibited slow degradation in physiological conditions, suggesting potential applications as implants that would be gradually replaced by organically grown lung tissue.
The ability to create 3D models via this bioink opens yet another frontier in lung disease research. These models could facilitate deeper investigations into disease mechanisms, enabling scientists to evaluate therapeutic strategies and the efficacy of new drugs without relying solely on animal models. As a result, this technique may significantly enhance the understanding of lung biology and the development of innovative treatments.
The implications of this research resonate far beyond the laboratory. If further developed, the mucus-based bioink has the potential to transform the landscape of lung disease treatment and research. By enabling a more accurate modeling system, it could inspire breakthroughs in personalized medicine, where therapies can be tailored to the individual characteristics of a patient’s lung disease.
This advancement not only represents a leap forward in bioprinting technology but also embodies hope for millions burdened by chronic lung conditions. As researchers continue to explore and refine this technology, the prospect of improved outcomes for lung disease sufferers becomes increasingly tangible.