The recent modeling study published in JAMA has sent shockwaves through public health circles, highlighting the chilling potential for a resurgence of measles in the United States. The study indicates that recent declines in childhood vaccination rates could lead to catastrophic public health consequences, as diseases once thought to be subdued may soon reignite. This report isn’t merely a statistic-laden warning; it embodies a collective responsibility to safeguard the health and safety of our communities. The grim projection of 850,000 annual measles infections coupled with over 2,500 deaths paints a vivid picture of what is at stake if we fail to act.
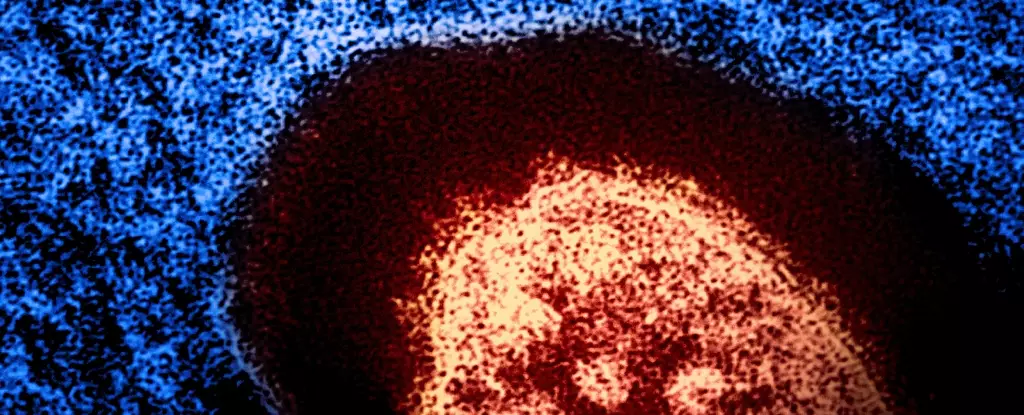
Historically, measles has been one of the most contagious diseases on the planet, capable of infecting 12 to 18 individuals from just one infected person. Compared to other infectious diseases like influenza or COVID-19, measles demonstrates a far more aggressive transmission pattern. This virulence makes the urgency of achieving herd immunity even more daunting. To effectively prevent the spread of this dangerous virus, it is crucial that at least 95% of the population be vaccinated. Yet the current vaccination landscape shows alarmingly low numbers, both in the U.S. and globally.
The Epidemiological Landscape: A Global Concern
The troubling statistics aren’t confined to the United States alone. Even in developed nations like England, vaccination rates for the measles, mumps, and rubella (MMR) vaccine are falling. With less than 84% of five-year-olds having received both doses, questions arise about the long-term implications for herd immunity. Countries that have successfully eradicated measles now face the frightening prospect of these diseases making a catastrophic comeback, reminiscent of the pre-vaccine era.
The overall health implications of measles are deeply concerning. One in five children affected by measles require hospitalization, and complications such as pneumonia and encephalitis pose further risks. With the potential for measles to claim the lives of up to three in every 1,000 affected children, the stakes are profound. This risk is not isolated to measles; a decline in vaccination rates can lead to a resurgence of other dangerous diseases, including rubella—known for causing severe birth defects—polio, which results in paralysis, and diphtheria, which can be fatal in many unvaccinated children.
Understanding the Roots of Vaccine Hesitancy
So, what has contributed to the plummet in vaccination rates? A multitude of factors lies at the root of vaccine hesitancy, ranging from disruption caused by the COVID-19 pandemic to the pervasive misinformation propagated through social media. The COVID pandemic triggered the most significant drop in global vaccination coverage in 30 years, and many regions are still grappling with the aftermath. Conflict zones and natural disasters have only exacerbated the situation, highlighted by Yemen’s staggering report of over 10,000 measles cases within just six months.
Misinformation also plays a significant role in vaccine hesitancy. Claiming a linkage between the MMR vaccine and autism, a notion rooted in a now-debunked study from 1998, continues to erode public confidence. Despite overwhelming evidence and numerous reliable studies dismissing this claim, misconceptions linger on through social media, effectively acting as an obstacle to informed decision-making among parents. The World Health Organization has recognized this misinformation campaign as a critical danger to global health, highlighting the urgent need to combat these persistent falsehoods.
The Responsibility of Public Health and Community Engagement
Navigating the complex landscape of vaccine information requires careful thought and engagement from healthcare professionals, parents, and community leaders alike. Exploring the multifaceted reasons behind vaccine hesitancy is part of this crucial dialogue. Parents naturally deliberate the risks and benefits regarding their children’s health, but it is imperative to focus not only on their own child but also on communal obligations. Fluctuations in vaccination rates compromise herd immunity, endangering those vulnerable individuals who cannot be vaccinated due to medical conditions or age, such as infants under a year old.
As public health advocates, it is essential to rally for vaccination. Diseases like measles do not adhere to notions of time or geographical confines; they thrive where there are gaps in immunity. The flames are already kindling; without immediate action to raise vaccination rates and rebuild trust in vaccines, we risk witnessing a public health crisis that will have profound implications for future generations. Vaccination remains a potent tool in our arsenal against the resurgence of such infectious diseases, and igniting a renewed commitment to immunization can help extinguish the embers before they ignite into an uncontrollable wildfire.