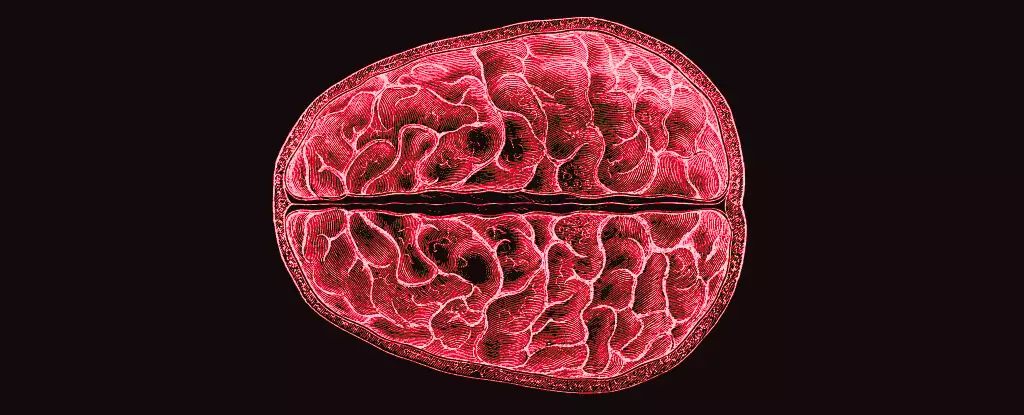
The menstrual cycle is one of nature’s profound biological rhythms, orchestrating not just reproductive processes but also affecting various aspects of physical and mental health. Recent research led by neuroscientists Elizabeth Rizor and Viktoriya Babenko at the University of California, Santa Barbara dives deep into an area less discussed—how hormonal fluctuations throughout the menstrual cycle intricately reshape brain structure. It is stunning to think that research has often overlooked this link, treating hormonal changes primarily as mere side notes in the narrative concerning cognition rather than taking center stage. The study’s findings emphasize that hormonal variations can lead to significant transformations in brain microstructure, urging us to reevaluate our understanding of menstruation’s complexities.
Research Breakthroughs and Their Implications
The 2023 study captures the nuances of the menstrual cycle by closely tracking 30 women through its various phases: menses, ovulation, and mid-luteal. By leveraging advanced MRI technology, the researchers measured not just the participants’ hormone levels but also detailed the structural changes occurring in both gray and white matter throughout each menstrual phase. The revelations are astounding; rather than observing changes confined solely to the hypothalamic-pituitary-gonadal-axis regions, researchers noted brain-wide transformations. This kind of comprehensive investigation sheds light on the reality that hormonal shifts enact far-reaching impacts on brain structure, reinforcing the observation that the brain’s architecture is as dynamic as the hormones that govern the cycle itself.
The Call for Greater Research and Awareness
It’s bewildering, given that menstruation affects half the population for significant portions of their lives, to realize how little comprehensive research exists in this area. Much of what we do know has historically been relegated to cognitive functions—how women perform through various tasks during different hormonal phases—rather than directly assessing how hormonal fluctuations alter the foundational structures themselves. The study’s authors contend, “Cyclic fluctuations in HPG-axis hormones exert powerful behavioral, structural, and functional effects…” clearly indicating a need to shift focus from behavioral patterns to structural changes in an effort to fully understand the menstrual cycle’s complexities.
By identifying how hormones like estradiol and progesterone influence brain changes, we begin to eliminate the menstruation gap in neuroscience. The documented relationship between hormonal fluctuations and white matter microstructure unlocks possibilities for future investigations into atypical mood swings or severe mental health issues related to the menstrual cycle. Current literature has largely neglected to connect the physical anatomy of the brain with these common yet debilitating phenomena, and the implications could be transformative for mental healthcare strategies for those affected.
Impacts on Daily Life and Societal Perception
The ramifications of this research extend beyond academic interest into the realm of real-world applications and societal attitudes towards menstruation and women’s health. For generations, menstruation has existed in a shroud of stigma and misunderstanding, labeled as a mere inconvenience rather than a complex interaction of biological processes with cognitive and emotional functions. By elevating discussions surrounding the menstrual cycle and acknowledging its multifaceted impact on women’s health, society can dismantle long-standing misconceptions. Greater awareness could lead to increased support for those who suffer from premenstrual dysphoric disorder (PMDD) and other hormonally-related mental health concerns.
Furthermore, recognizing the brain’s dynamic nature during menstruation could inform therapeutic practices and enhance approaches toward mental health care tailored to women’s unique needs. As we unravel the interplay between hormones and brain structure, the potential for personalized treatments becomes evident.
Charting a New Course in Women’s Health
This groundbreaking research not only lays a cornerstone for further studies but also fosters a broader dialogue about the relevance of menstruation in the context of brain health. What we are beginning to uncover is a layered tapestry that connects hormonal changes to neurological changes, which in turn could catalyze changes in how we approach women’s mental health holistically. As this field of research evolves, it becomes increasingly critical for societal attitudes to adapt accordingly—recognizing the vital, impactful role that menstruation plays, not just as a biological process, but as an intrinsic component of female identity and well-being.