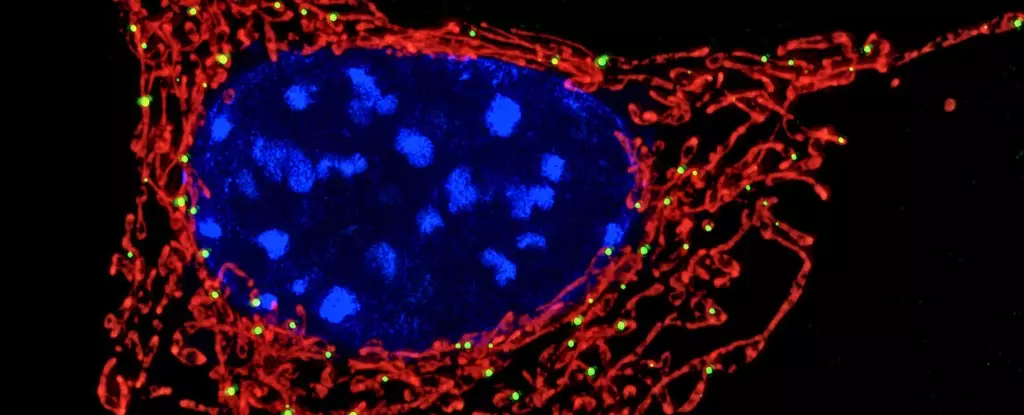
For decades, mitochondria have been pigeonholed as the energy factories of the cell—tiny but critical organelles whose primary job is to convert nutrients into usable energy. This simplistic view, however, grossly underestimates their far-reaching importance. Emerging research is dramatically reframing mitochondria as dynamic regulators of immune function, inflammation, and cellular fate. Most striking among recent discoveries is their direct involvement in sensing bacterial threats and orchestrating immune defenses, particularly through their interplay with neutrophils, the body’s frontline white blood cells.
Mitochondria and Neutrophils: A New Immunological Dialogue
Neutrophils are the immune system’s first responders, rushing to infection sites and deploying an arsenal of weapons to neutralize invading pathogens. One of their remarkable defenses is the formation of neutrophil extracellular traps (NETs)—sticky, web-like matrices composed of DNA spun with antimicrobial proteins. These NETs ensnare bacteria, preventing their spread and making them easier targets for destruction by other immune cells.
Previously, the scientific consensus held that NET production was mainly triggered by cellular injury or stress signals, a somewhat passive response to infection. However, a groundbreaking study uncovers a far more sophisticated mechanism: mitochondria within neutrophils sense bacterial metabolites, notably lactate, produced during infection. This signaling triggers the deployment of NETs, demonstrating mitochondria’s role as vigilant sensors that decode microbial metabolic cues to mobilize a targeted immune response.
Decoding Bacterial Signals Inside the Cell
The revelation that mitochondria can detect bacterial lactate inside neutrophils is both unexpected and fascinating. Bacteria, during their own metabolic processes, release lactate—a molecule more commonly linked with muscle fatigue in humans. When neutrophils engulf bacteria into a specialized compartment called the phagosome, the mitochondria somehow sense this lactate despite the physical separation between organelle and bacterium.
This mitochondrial sensing acts as a critical alert system. It signals when initial intracellular killing mechanisms aren’t fully effective, prompting neutrophils to release NETs and trap bacteria extracellularly. This sophisticated interplay underlines an exquisite level of cellular communication and coordination that challenges existing models of immune function.
The Implications for Autoimmune Diseases and Infection Susceptibility
These insights have clinical implications, especially for autoimmune disorders like systemic lupus erythematosus (SLE). Paradoxically, lupus patients experience overactive immune systems but remain vulnerable to infections. Researchers have traced this vulnerability back to faulty mitochondrial lactate sensing in neutrophils. In lupus, defective mitochondrial function disrupts NET formation, sabotaging the neutrophils’ ability to trap and neutralize pathogens effectively.
This duality—where immune overactivation coincides with impaired microbial defense—highlights mitochondria’s pivotal role in immune balance. They act not only as signal processors for mounting attacks but also as moderators to prevent immune system misfires that damage host tissues.
Transforming Immunometabolism Into Therapeutic Potential
The emergent concept of immunometabolism—that metabolism and immune responses are deeply interwoven—positions mitochondria as central arbiters of immune decisions. Recognizing mitochondria as more than bioenergetic hubs allows researchers to envision exciting therapeutic avenues. Enhancing mitochondrial sensitivity could potentially boost NET formation in patients with compromised immunity, such as those with lupus or other chronic infections.
Conversely, in diseases where NETs exacerbate tissue damage, such as certain autoimmune conditions or severe COVID-19 cases, modulating mitochondrial signals to temper NET release might reduce harmful inflammation and collateral tissue injury. This bidirectional therapeutic potential underscores the nuanced role mitochondria play in both defending and sometimes inadvertently harming the host.
Charting Future Courses: The Mitochondrial Frontier in Immunity
The discovery that mitochondria can sense microbial metabolites signals only the beginning of unraveling the immune system’s metabolic intelligence. Are other immune cells equipped with similar mitochondrial sensors? Do different bacterial byproducts serve as molecular beacons, influencing immune decisions in untold ways? These questions open vast investigative avenues.
Far from being passive energy factories, mitochondria emerge as vigilant watchtowers—constantly monitoring subtle biochemical signals within the cellular landscape to orchestrate precise immune responses. This evolving understanding challenges traditional immunology and invites a recalibration of how we study and manipulate immune function in health and disease. Embracing mitochondria’s multifaceted role could revolutionize treatments that finely tune immune activity, curtail infections, and mitigate autoimmune damage with unprecedented accuracy.