For years, the fight against obesity has heavily relied on medications such as Ozempic, which mimic the hormone GLP-1 to suppress appetite and regulate blood sugar levels. While these drugs have proven to be effective, they come with drawbacks, including side effects and the need for continuous medication. However, a groundbreaking shift is underway. Recent research suggests that leveraging our gut microbiome—the trillions of microorganisms residing in our intestines—might provide a more natural, sustainable pathway to weight management. Unlike synthetic drugs, enhancing the body’s innate mechanisms could lead to profound, lasting health benefits.
Previous efforts to boost GLP-1 production focused on directly stimulating hormone release through pharmaceuticals. Though helpful, this approach often ignores the complex biological interplay within our digestive system. The latest studies, however, reveal that the gut’s own microbiota can produce byproducts capable of stimulating the same hormone—GLP-1—potentially revolutionizing our approach to combating obesity. This shift from medication to microbiome-centric therapies offers the promise of more holistic health solutions that work harmoniously with our bodies’ natural processes.
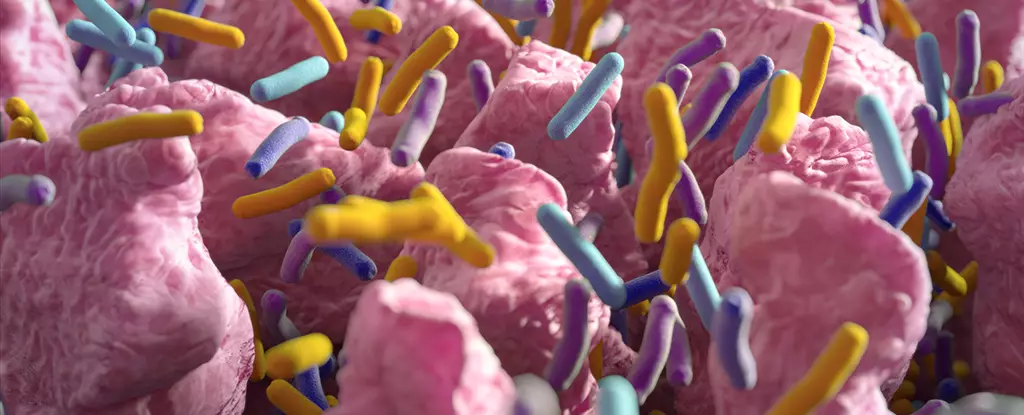
The Gut Microbiome: The Hidden Powerhouse in Metabolism
The notion that our gut microbes can influence weight is not entirely new, yet the mechanisms remained elusive until recent advances. Enteroendocrine cells (EECs)—specialized cells scattered along the intestinal lining—are responsible for producing and releasing hormones like GLP-1 in response to food intake. Studies from Marshall University have identified a deficiency of these cells as being linked to obesity, hinting at a biological shortfall that could be corrected.
The latest research makes a compelling case: by supplying specific microbial metabolites, such as indole derived from the amino acid tryptophan, we could stimulate the growth of EECs. Tryptophan-rich foods—like poultry, eggs, and cheese—may, therefore, harbor untapped potential as natural dietary tools that support weight loss. The fascinating discovery is that these metabolites activate the aryl hydrocarbon receptor (AhR) within intestinal cells, triggering a biological cascade that leads to increased production of EECs and consequently, more GLP-1.
This insight elegantly ties nutrition, microbiology, and endocrinology together, suggesting that diet alone could influence our hormonal balance far more profoundly than previously appreciated. It also underscores the importance of personal microbiome health. Different microbial compositions in individuals could explain why some people respond better to diet or microbiome-targeted therapies than others.
From Lab Discoveries to Personal Health Solutions
While translating these findings into practical treatments remains a challenge, their implications are profound. Imagine a future where personalized nutrition or probiotic regimens enhance your gut’s ability to produce its own weight-regulating hormones—a stark contrast to the reliance on pharmaceuticals with undesirable side effects.
The potential here is to develop dietary supplements, probiotics, or even targeted compounds that activate specific receptors like AhR. Such approaches could restore EEC populations naturally, reducing dependence on drugs like Ozempic and addressing one of the core issues in obesity—hormonal imbalance rooted in our gut.
However, it’s crucial to recognize the gap between animal models and human applications. The complexity of human microbiomes and individual variability means that what works in rats or lab-grown organoids might not have a straightforward translation to human treatment. Nevertheless, this research opens an exciting door: harnessing the symbiotic relationship between diet, microbiota, and hormonal health to create more sustainable solutions.
In the long run, this approach aligns with a broader philosophy of empowering the body’s innate healing capabilities. As science progresses, we might see a paradigm shift—viewing weight management less as a battle against our biology and more as a partnership with it. Though treatments based on gut microbes are still under investigation, their potential to redefine how we approach obesity and metabolic health is undeniable. This is not merely about another pill; it’s about reimagining our relationship with our bodies and the microscopic partners that live within us.