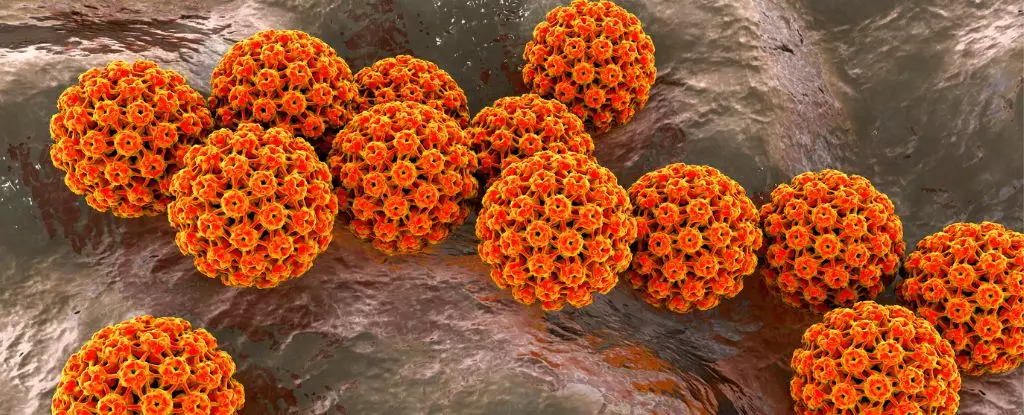
Recent research has shed light on the concerning reality that men remain at risk for potentially dangerous strains of human papillomavirus (HPV) throughout their lives. This insight is crucial, as the study points out that cases of oropharyngeal cancer—which develop in the throat and mouth—are on the rise, especially among men who lack other common cancer risk factors. The significance of this research extends beyond academic interest; it serves as a clarion call for improved vaccination coverage, particularly targeting middle-aged men who may have missed early opportunities for protection.
The Rising Tide of Oropharyngeal Cancer
Oropharyngeal cancers have reached alarming levels in specific regions, such as the United States and Europe. The troubling trend is that men are diagnosed far more frequently than their female counterparts, even in the absence of lifestyle risk factors like smoking or excessive alcohol consumption. The evidence gathered from studies conducted in the U.S., Brazil, and Mexico indicates that HPV, particularly cancer-causing strains, is driving this surge in cases. Notably, the study encompassed a diverse group of 3,137 healthy men aged between 18 and 70, revealing a consistent risk of acquiring hazardous HPV strains regardless of age.
While HPV is commonly understood as a sexually transmitted infection, the modes of transmission are more diverse than previously recognized. Strains known to be linked to oral cancers, notably HPV-16 and HPV-18, are present in roughly 90% of these cancer cases. Fortunately, vaccines are available that effectively shield against these specific strains; however, vaccination rates for young males significantly lag behind those of young females. This discrepancy in vaccination raises critical questions about public health strategies, particularly since the incidence of oropharyngeal cancer continues to escalate while cases of cervical cancer decline.
The Centers for Disease Control and Prevention (CDC) recommends that all young individuals up to age 26 receive the HPV vaccine to safeguard against various cancers. However, for those over this age, the vaccine is largely restricted to males with compromised immune systems or other risk factors. The CDC suggests that the benefits of vaccination diminish after age 26 due to the likelihood of prior exposure to HPV. This prevailing assumption, however, may need reevaluation in light of recent findings that challenge its validity.
Historically, research into the long-term risks of oral HPV infections in men has been limited and often targeted specific demographics, such as men who have sex with men. Yet, the pathways for contracting oral HPV extend beyond sexual interactions, suggesting a broader range of potential exposure. Study authors from the Moffitt Cancer Center emphasize the necessity for continual vigilance against oral HPV, particularly given their findings that established a consistent risk of infection across different ages.
In their study, they collected oral gargle samples from participants on multiple occasions between 2007 and 2016, finding that nearly 20% had existing oral HPV infections, with around 6% exhibiting strains known to cause cancer. Such data underlines the pressing need for tailored vaccination strategies that reach not only younger populations but also those who may have missed previous opportunities.
The study highlights several risk factors associated with the acquisition of HPV-16, including alcohol consumption and sexual behavior. As men age, the likelihood of developing cancers associated with HPV-16 progressively increases, emphasizing the importance of early intervention and preventive measures. Public health policies must adapt to these findings by enhancing education and awareness regarding oral HPV risks and expanding access to vaccines for all eligible demographics.
The landscape of oral HPV and its implications for men’s health calls for a significant shift in both public awareness and vaccination strategies. Ensuring that every individual is informed about the risks and benefits of vaccination, regardless of age, is essential for combating the epidemic of oropharyngeal cancers linked to HPV. Acting decisively now could change the trajectory of HPV-related health outcomes, ultimately saving numerous lives in the future.