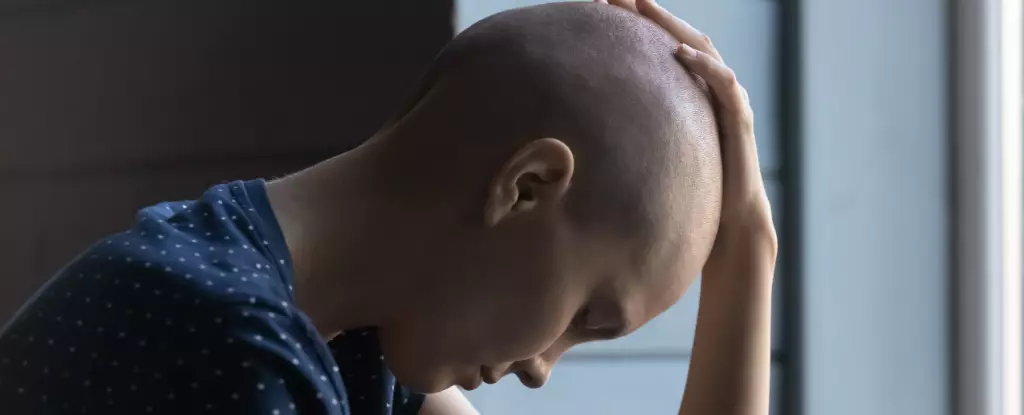
Cancer, an insidious and multifaceted disease, has profound effects not only on the body but also on the psychological state of its patients. One of the most devastating consequences of advanced cancer is cachexia, a syndrome that primarily manifests as extreme muscle wasting and unintended weight loss, often striking around 80% of patients in late stages of the disease. What many might overlook is the accompanying psychological toll, characterized by a profound loss of motivation and apathy toward activities that were once cherished. This emotional detachment signals more than just a response to physical decline; it raises questions about the intricate connections between inflammation, brain circuitry, and motivation.
As patients grapple with diminishing physical capabilities, they often withdraw from social interactions and treatment regimens, creating an isolating cycle of despair not just for themselves, but also for their families who feel helpless as they watch a beloved sufferer retreat into a shell. Traditionally, healthcare providers have viewed these symptoms as a natural emotional reaction to the disease. However, recent research is challenging this narrative. The rising evidence suggests that this apathy might actually stem from biological processes triggered by cancer itself, transforming what seems like a psychological issue into a symptom of disease pathology.
The Neuroscience Behind Motivation and Apathy
Recent studies illuminate how cancer, particularly through its inflammatory byproducts, may hijack vital brain circuits responsible for motivation. By leveraging advanced neuroscience tools, researchers have been able to draw a clearer picture of the biological mechanisms behind cancer-induced apathy. Specifically, a small yet crucial region of the brain known as the area postrema has been pinpointed as a primary player in this cascade of motivational decline. Remarkably, this region, which significantly lacks a traditional blood-brain barrier, serves as an inflammation detector, effectively sampling inflammatory signals circulating through the bloodstream.
In the face of a growing tumor, these inflammatory markers trigger a complex neural cascade that ultimately diminishes dopamine levels, which are integral to the brain’s motivation and reward pathways. Dopamine is often misconceptualized as merely a “pleasure chemical,” but its role transcends mere enjoyment—it’s a critical element in our willingness to engage with challenging tasks. The erosion of dopamine levels can severely impair one’s desire to pursue even simple rewards, leading individuals to abandon efforts that might prove beneficial or rewarding.
Observational studies utilizing mouse models reveal actionable insights into these phenomena. Experimental tasks designed to measure effort demonstrated that while mice would aggressively seek out easily attainable rewards, they readily retreated from challenges requiring more substantial effort. This mirrors starkly with real human experiences where patients frequently articulate feelings of overwhelming hardship in undertaking even basic tasks.
Hope on the Horizon: Therapeutic Interventions
Intriguingly, the research points to potential avenues for therapeutic intervention—ways to reignite motivation even in the face of relentless disease progression. By finetuning the interaction between inflammatory factors and the brain’s motivational circuitry, scientists have observed improvements in behavior among affected mice. Simple manipulations, such as disabling certain neurons in the area postrema or administering anti-inflammatory drugs, have demonstrated promising results in restoring lost motivation.
These findings highlight not only the necessity for more effective treatments targeting cancer cachexia but also the potential to extend these therapeutic strategies to manage other inflammation-driven conditions, such as rheumatoid arthritis and chronic fatigue syndromes. The inflammatory mechanisms that underpin apathy in various chronic diseases could be addressed, allowing patients a chance to reclaim their zest for life despite ongoing health challenges.
Furthermore, this research reinforces a paradigm shift in how we view the interplay between physical and psychological symptoms. It challenges the oversimplified divide, urging healthcare practitioners to adopt a more holistic perspective that acknowledges the role of inflammation within the broader behavioral and emotional landscape of disease.
The Broader Implications of Motivation Loss
In understanding the pathways linking inflammation to motivation loss, we hold the potential to unlock not just hope for cancer patients but also for a broader population suffering from chronic illnesses. Recognizing that apathy may originally serve as a protective mechanism in response to acute infection, we see the darker flipside of this evolutionary adaptation—prolonged apathy in the face of chronic illness can deepen human suffering and compromise quality of life.
Efforts to intercept the signals that lead to motivational decline could facilitate reclaiming dignity and engagement for patients. As we push forward with research that combines neuroscience and oncology, we inch closer to a future where patients might not only survive cancer, but thrive emotionally and psychologically—even while battling the relentless tides of disease. Such advances could redefine standards of care and significantly alter the quality of life for countless individuals.
The potential to restore shattered motivation affirms a universal truth: even in the depths of adversity, the desire to connect, to strive, and to live profoundly enhances the human experience. This promise of engagement, even amidst profound illness, offers a beacon of hope in the dark maze of chronic disease.