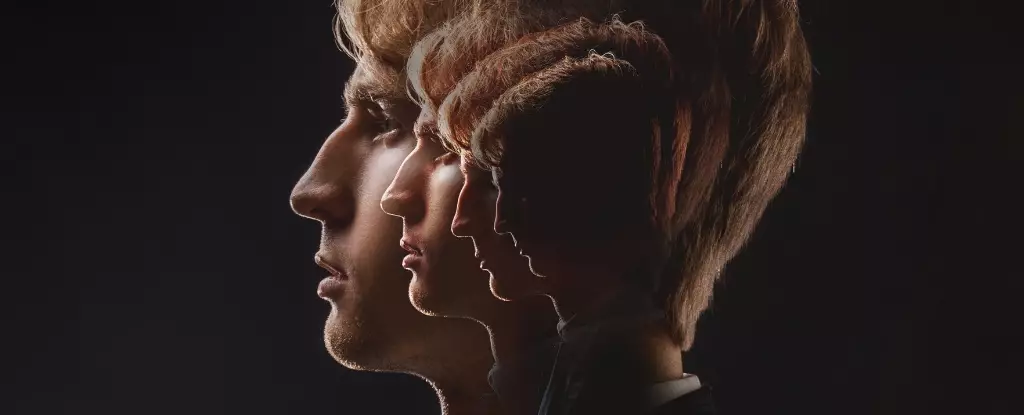
Schizophrenia is far more than a mere mental health condition; it’s a severe and often debilitating illness that afflicts over 20 million individuals globally. This disorder is notorious for its profound impact on perception, thought, and behavior, frequently manifesting through vivid hallucinations and persistent delusions. Understanding the roots of schizophrenia requires delving into a complex web of neurobiology, psychological factors, and socio-environmental influences that come to light particularly during the transformative period of adolescence to early adulthood. Amidst this complexity, new research suggests that accelerated brain aging is not just a side note but a core component driving the onset and progression of schizophrenia.
Brain Development and Neurodegeneration
Current academic discourse suggests that schizophrenia arises from multifactorial contributors, including notable changes in brain development during critical life stages. Emerging theories posit that these changes may intersect with already established neurodevelopmental disorders like dyslexia and autism. However, groundbreaking research is illuminating a unique biological marker that could revolutionize our understanding of schizophrenia: the neurofilament light protein (NfL). This biomarker, released into the bloodstream when neurons sustain damage, serves as a tangible measure of neuronal health.
The relationship between NfL and schizophrenia indicates a troubling trend wherein individuals diagnosed with the disorder may experience not just typical neurodegeneration but an accelerated form of brain aging. Instead of the gradual deterioration typically observed with normal aging, the rise in NfL suggests that schizophrenia may be akin to living under chronic neurotoxic conditions, leading to premature decline.
Understanding Neuronal Injury
To grasp the implications of elevated NfL levels, it is critical first to understand neuronal injury—the damage to the specialized cells that facilitate communication within the brain and nervous system. Impaired neurons can lead to varying neurological symptoms, depending on their location and extent of damage. This distinction becomes particularly poignant when discussing schizophrenia, where the manifestations of neuronal decline are not only more severe but occur at a markedly accelerated rate compared to healthy individuals of the same age.
The stark contrast between normal and pathological brain aging is crucial. While a typical older adult might experience mild forgetfulness or slower reaction times without significant impairment, individuals with schizophrenia often face debilitating cognitive deficits. This revelation underscores the urgency for early intervention and proactive treatment strategies that focus not just on managing symptoms but on addressing the underlying biological mechanisms of the disorder.
The Broader Health Implications
Individuals enduring schizophrenia frequently grapple with a myriad of compounding health challenges that exacerbate their condition. Research indicates that these individuals often experience a diminished lifestyle quality, marked by social isolation, high unemployment rates, physical inactivity, and increased likelihood of substance abuse. Alarmingly, it has been estimated that people with schizophrenia may have a life expectancy 20-30 years shorter than their peers, largely due to chronic age-related diseases such as cardiovascular issues and cancer.
One contributing factor to these poor health outcomes is the prevalence of comorbid conditions, with approximately half of all individuals with schizophrenia facing at least one additional chronic medical issue. The relationship between mental health and physical health becomes apparent here, as lifestyle choices such as smoking and poor diet are often coping mechanisms for distressing psychological symptoms.
Implications for Treatment and Research
As researchers explore the biological underpinnings of schizophrenia, the findings surrounding NfL may illuminate not only avenues for effective diagnosis but also new strategies for treatment. If changes in NfL correlate with accelerated aging processes in the brain, this could allow for more personalized approaches tailored to the patient’s unique biological profile.
Furthermore, understanding the metabolic and lifestyle challenges facing individuals with schizophrenia can lead to comprehensive interventions. For instance, addressing aspects of physical health through tailored exercise regimens, proper nutrition, and social support networks could mitigate some of the accelerated aging mechanics being observed.
It is essential to recognize that the journey to understanding schizophrenia is far from over. The ongoing investigation into biomarkers like NfL opens up exciting possibilities for early detection and improved therapeutic strategies, providing hope for a better quality of life for millions grappling with this complex disorder. As science evolves, so too must our approach to mental health, shifting from reactive care to proactive, integrative methodologies that encompass both mind and body.