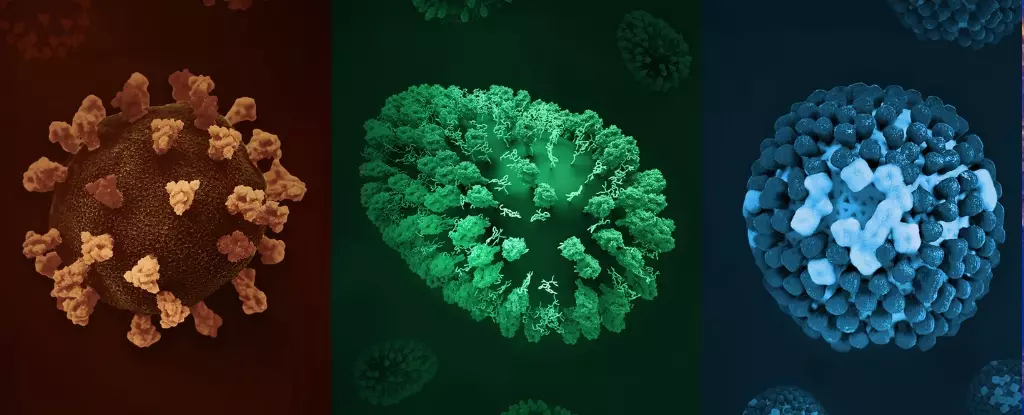
In the intricate dance of infectious diseases, the reproductive number, commonly known as R0 or R-nought, emerges as a key metric that determines a pathogen’s capacity to spread. Far from being just a scientific statistic, R0 embodies the essence of epidemic potential. It quantifies the average number of secondary infections generated by a single infected individual in a wholly susceptible population. This seemingly simple number holds profound implications: an R0 above one signals a likelihood of exponential growth, while a value below one indicates the disease will eventually wane and disappear.
Understanding R0 is not a mere academic exercise; it’s a fundamental insight that shapes our response strategies. Diseases with high R0 values, like measles, demonstrate how swiftly infections can cascade through communities if unchecked. Conversely, illnesses with lower R0 figures, such as tuberculosis, remind us that even less contagious pathogens pose significant threats, especially when neglected or inadequately treated. Grasping the significance of R0 empowers public health officials to design targeted interventions—be it vaccination, contact tracing, or social distancing—to disrupt transmission chains effectively.
The Contagious Titans: Measles and Its Global Resurgence
Among the universe of infectious diseases, measles stands out as an exemplar of contagiousness, with an astonishing R0 spanning from 12 to 18. To put that into perspective, one infected individual can potentially infect dozens—sometimes hundreds—of others. The implications are chilling: a single unvaccinated person entering a community with low immunization rates can spark a rapid, expansive outbreak.
What makes measles particularly alarming is its mode of transmission—tiny airborne droplets that can stay suspended and infectious for hours. This airborne nature bypasses the need for direct contact, enabling infection even in spaces where symptomatic individuals have already left. The disease’s stealth is compounded by the fact that infected persons can spread it before showing symptoms, compounding the difficulty in containment.
Recently, measles has been making an unwelcome comeback in parts of the world that once considered it eradicated. Declines in vaccination rates—exacerbated by misinformation, vaccine hesitancy, and pandemic-related disruptions—have created fertile ground for outbreaks. This resurgence underscores a brutal truth: herd immunity is fragile. When vaccination coverage dips below the critical threshold (~95%), even diseases with high R0 values can swiftly exploit the vulnerability, turning communities into vectors of disease.
Silent but Deadly: Diseases with Lower R0 and Their Persistent Threats
While the spotlight often falls on highly contagious pathogens, diseases with modest R0 values can be equally devastating—particularly in populations with inadequate healthcare or poor living conditions. Tuberculosis (TB), for example, has an R0 usually less than one in optimal conditions but can climb up to four in overcrowded environments. Its slow transmission is a double-edged sword; the disease often remains hidden for months or years before manifesting symptoms, allowing it to silently spread through close contact.
TB’s true menace lies not in its contagiousness alone but in the complexity of its treatment. Once infected, eliminating TB requires a painstaking course of multiple antibiotics over at least six months. The emergence of drug-resistant strains further complicates containment, transforming what might have been manageable infections into formidable public health crises. The pathogen’s tenacity exemplifies how even less contagious diseases can persist and cause significant harm if left unchecked.
In contrast, Ebola, with an R0 of 1.5 to 2.5, highlights how high fatality does not necessarily correlate with high transmission rates. Its spread hinges on intense physical contact with bodily fluids, often during caregiving or traditional funeral rites. Despite its lower R0 compared to measles, Ebola’s high mortality rate makes it a formidable threat, especially in settings with inadequate healthcare infrastructure.
The Power of Prevention: Vaccination and Herd Immunity as Shields
Prevention remains the cornerstone of infectious disease control, and vaccination is arguably the most effective tool in our arsenal. It’s a strategy rooted in communal responsibility, aiming not only to protect the vaccinated individuals but also to create an immune barrier—herd immunity—that slows or halts transmission altogether.
Achieving herd immunity thresholds is particularly critical for protecting the most vulnerable—infants, pregnant women, immunocompromised individuals—who cannot receive certain vaccines. When enough people are immunized, the pathogen encounters an insurmountable challenge in finding new hosts, effectively reducing the R0 below the critical level needed for sustained spread.
Yet, vaccination efforts face hurdles—misinformation, cultural resistance, logistical challenges—that threaten to undermine collective immunity. The recent resurgence of measles epitomizes this danger. It serves as a stark reminder that diseases with high R0 are especially adept at exploiting gaps in immunization coverage. Ensuring widespread vaccination is not merely about individual protection; it is a moral imperative to shield those who are most susceptible and to prevent the emergence of future outbreaks.
Reevaluating Our Approach to Infectious Threats
The COVID-19 pandemic has thrust infectious diseases into the global spotlight, revealing both our vulnerabilities and our resilience. It has demonstrated that understanding the mechanics of disease transmission—particularly the pivotal role of R0—is vital in crafting effective responses. As some pathogens exhibit an alarming capacity to spread rapidly, others lurk silently, only to emerge under the right conditions.
In the end, our fight against infectious diseases hinges on a nuanced understanding of transmission dynamics. Recognizing which pathogens are most contagious and how they propagate informs not just immediate responses but also long-term strategies. A robust immunization infrastructure, widespread public education, and swift containment measures are our best tools to turn the tide against even the most formidable microbial foes. The lesson is clear: knowledge of infectious potential is power—and that power can save countless lives when wielded wisely.