Herpes simplex virus type 1 (HSV-1) is widely recognized as the primary cause of cold sores, but recent research illuminates its more insidious potential—its ability to infiltrate the brain and central nervous system (CNS). A notable study by researchers from the University of Colorado and the University of Bourgogne, France, investigates how HSV-1 manages to invade the brain, mapping the various affected regions and unveiling potential consequences. Previous knowledge hinted at the connection between HSV-1 and neurodegenerative disorders, particularly Alzheimer’s disease, but concrete pathways for viral invasion into the CNS have been vague until now.
The research underscores the importance of understanding HSV-1’s entry routes into the brain, which primarily occur through the trigeminal and olfactory nerves. Despite this knowledge, the internal processes that facilitate the spread within the CNS remain obscure. Neurologist Christy Niemeyer emphasizes the importance of elucidating the vulnerable regions of the brain for developing a comprehensive understanding of the pathogenesis associated with HSV-1 and related diseases.
Mapping the Affected Brain Regions
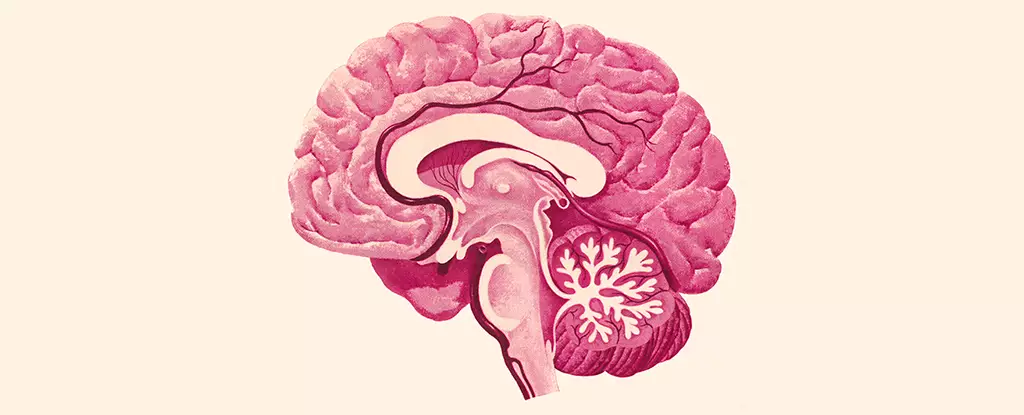
The findings of this study reveal that HSV-1 predominantly affects critical areas of the brain, such as the brain stem and hypothalamus. The brain stem, known for managing vital functions such as breathing and heartbeat, as well as coordinating sleep and movement, becomes a focal point for HSV-1 activity. Simultaneously, the hypothalamus, a pivotal region involved in regulating mood, appetite, and hormone balance, also experiences the brunt of viral intrusion.
Despite heavy impacts on these significant areas, it is crucial to note that certain brain regions remain relatively unharmed by the virus. Notably, the hippocampus—essential for memory formation and spatial navigation, and often linked to Alzheimer’s disease—seems to escape direct infiltration. Likewise, the cortex—responsible for various cognitive functions such as memory retention and focused attention—also remains unscathed. This selective targeting raises important questions about the specific vulnerabilities within the brain and their relevance to the long-term consequences of HSV-1.
In addition to mapping affected regions, the study offers insights into microglial behavior in response to HSV-1 infection. Microglia serve as the brain’s immune cells, and their activation appears to correlate with HSV-1 presence, demonstrating signs of inflammation in affected areas. Intriguingly, even after the viral presence has subsided, these immune cells continue to exhibit heightened activity, indicating a prolonged inflammatory reaction.
Neurologists have long understood that persistent inflammation is detrimental, potentially leading to severe outcomes, such as encephalitis—the widespread inflammation of the brain. While the study did not evidence full-blown encephalitis in the subjects, the ongoing inflammatory state highlighted raises concerns about cumulative damage and functional impairments in the affected brain regions.
The implications of this research extend beyond understanding HSV-1’s behavior within the CNS; it poses significant questions about its relationship with neurodegenerative diseases like Alzheimer’s. Growing evidence suggests that HSV-1 may contribute to the onset or progression of such disorders through the inflammatory responses it elicits. The findings draw parallels between the regions impacted by both HSV-1 and Alzheimer’s, proposing the possibility that the mechanisms of damage may bear similarities.
Niemeyer’s assertion about chronic inflammation acting as a known trigger for various neurological diseases is particularly noteworthy. If HSV-1 encourages a state of persistent inflammation, this could contribute directly or indirectly to the neurodegenerative processes seen in conditions like Alzheimer’s. Understanding this relationship opens up avenues for further exploration into therapeutic strategies that could mitigate the impact of HSV-1 on the brain.
The study on HSV-1 serves as a critical step in unraveling the complex interactions between viral infections and neurodegenerative diseases. By comprehensively mapping affected brain regions, analyzing microglial responses, and elucidating the potential for chronic inflammation to incite lasting harm, researchers lay the groundwork for future explorations. As the scientific community strives to connect the dots between HSV-1 and conditions like Alzheimer’s disease, the ongoing pursuit of knowledge will undoubtedly inform innovative strategies for prevention and treatment, underscoring the intricate relationship between viral infections and neurological health.